LONDON - Gastrointestinal disorders have a wide range of causes but can be very difficult to treat effectively. Specialists at the Royal College of Physicians Annual Conference in London discussed the role of the nervous system and gut microbes in gastrointestinal disorders, and practical approaches to treating them.
Don’t Neglect Nervous Connections
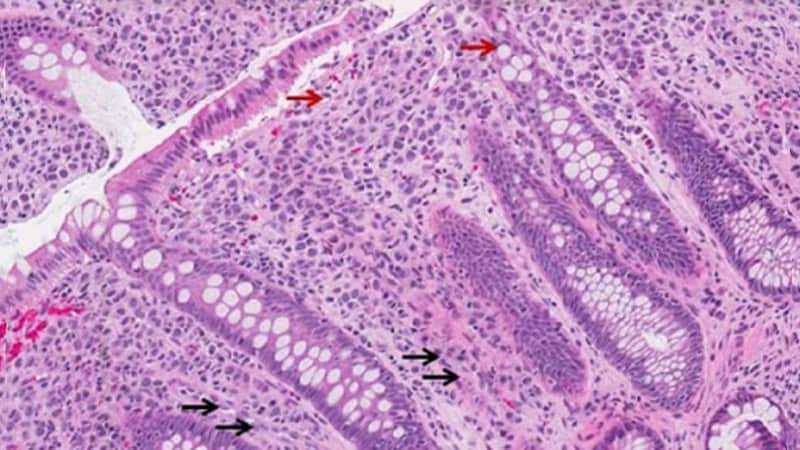
Consultant gastroenterologist Dr Peter Paine of Salford Royal Hospital said the role of the nervous system in gut disorders has been neglected, and suggested that these conditions could be treated more effectively if the neurological dysfunction is taken into account.
For example, chronic pancreatitis involves neuropathic and nociplastic mechanisms that can sensitise the nerves innervating the skin, viscera, and pancreas. It can also cause central sensitisation in the dorsal horn of the spinal cord. These changes hypersensitize the pain pathway, increasing the pain signals transmitted to the brain, and also cause allodynia, in which normally innocuous stimuli become painful.
Using quantitative sensory testing to measure pain thresholds to electrical and pressure stimulation can determine exactly where these processes have occurred, and predicts the efficacy of the analgesic effect of pregabalin in patients with chronic pancreatitis. Patients with lower pain thresholds in the Th10 dermatome compared to a control area are more likely to benefit from pregabalin treatment, compared with those who demonstrate no difference in thresholds.
Paine discouraged surgery and the use of opioid painkillers for treating chronic abdominal pain, as both can exacerbate patients' pain in the long-term. Irritable bowel syndrome (IBS) is associated with a threefold increase in cholecystectomy rates, a twofold increase in hysterectomy and appendectomy rates , and increased rates of colon resection and back surgery. However, significant numbers of patients experience surgically induced neuropathic pain following these procedures.
Opioids typically cause constipation, and smaller numbers of patients develop narcotic bowel syndrome, or opioid-induced hyperalgesia, characterised by frequent or chronic abdominal pain that worsens with continued or increasing dosage of the drug.
Changes in Gut Bacteria
IBS and other gastrointestinal disorders typically involve dysbiosis, or a change in the composition of gut bacteria, which are now known to interact with the enteric and central nervous systems via the so-called gut-brain axis. They also release a wide range of neurotransmitters that regulate the immune and endocrine systems.
Gut bacteria also produce metabolites that play important roles in the digestive system, including maintaining the integrity of the gut barrier, regulating appetite, energy homeostasis, gut motility, and absorption of water, sodium, lipids, and vitamins. In IBS, altered bidirectional communication between the gut and brain lead to visceral hypersensitivity, motor dysfunction, and low-grade inflammation.
Spurred on by the success of treating recurrent C. difficile infections with faecal microbiome transplants, the pharmaceutical industry is developing microbiome-based interventions. Prebiotics and probiotics are non-targeted approaches that can produce a general improvement in gut microbial composition and function. Phage therapy and gene editing can modify microbial strains that produce specific metabolites.
A study published in 2017 showed that transplantation of faecal microbiota from patients with IBS alters gut function and behaviour in recipient mice. On the basis of these findings, there are now at least 8 randomised controlled trials of faecal transplants for IBS, but only three of these have shown efficacy in treating the anxiety, stress, and depression that are typically comorbid with the condition.
Gut microbe research is a rapidly growing field that promises to transform treatments for gastrointestinal disorders. Although the field is still in its infancy, some companies make exaggerated claims about the benefits of microbiome sequencing, and there is a large market for untested products.
“Probiotics do have a positive effect in IBS, but we still haven't pinned down which bugs [are beneficial], and we do see the unregulated commercial industry as a problem,” Paine told Medscape News UK. “Patients come in with fancy colour print-offs and say 'I've sent my poop off and they've said it's this bug. What do I do?'”
According to Dr Tanya Monaghan of the University of Nottingham, developing effective microbiome-based treatments will require linking clinical trials to basic research into mechanisms of action.
“The only way to progress this field is to marry clinical interventional trials with mechanistic studies,” Monaghan said. “Taking a James Webb telescopic approach is worth it, because this is our internal universe, and it is the next pipeline of drugs.”
Moheb Costandi is a freelance science writer based in London.

.webp) 2 weeks ago
7
2 weeks ago
7























 English (US)
English (US)