Rebecca Levy-Gantt, DO, says many of her patients going through menopause first turn to social media to relieve various symptoms, which is how she keeps up-to-date in the world of supplements and other products with little, if any, clinical utility: the ever-growing list of patches, collagen gummies, or even infrared mats designed to "recharge" a patient's body through electromagnetic pulses marketed as miracle cures for the woes of menopause.
 Rebecca Levy-Gantt, DO
Rebecca Levy-Gantt, DOEven more concerning to Levy-Gantt, an ob/gyn and menopause specialist in Napa, California, are products containing ingredients that may interact badly with other medications or are prescribed without the complete medical history of her patients.
"I have told people that when they see, hear, or someone tells them they can 'fix' menopause, they have to be more skeptical," Levy-Gantt said. "It seems like a lot of people want to 'do' menopause, there's all these" products, services, and marketing popping up online.
More than 1 million people go through menopause each year. And in 2024, how-to advice on managing the condition is a big business, rife with overpriced therapies and false promises. Social media is the gateway to much of that misinformation, and women are increasingly turning to this medium for help.
Primary care clinicians can help patients think critically about the motives of online influencers, parse through an abundance of questionable information, and extract the science from the hype, experts say.
After the Fact
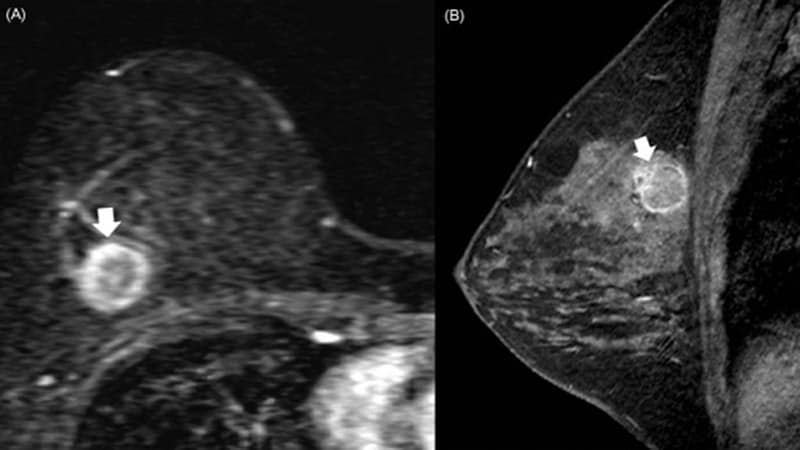
Through virtual health providers, several of Levy-Gantt's patients purchased hormone products that were touted on social media and online ads and subsequently developed uncontrolled menstrual bleeding, she said. Others received estrogen-only products despite having a uterus, risking estrogen-associated endometrial hyperplasia and increasing their risk for uterine cancer. Menopausal patients with uteruses should take combination estrogen-progestin therapy, according to clinical guidelines.
Other patients were swayed by influencers promoting the benefits of testosterone to improve libido and obtained high doses of the hormone through online clinicians. Too much of this drug can lead to side effects like weight gain, nausea, or increased cholesterol. Some patients consult levy-Gantt before going the telemedicine-only route, like in the case of a woman who requested a medication for menopause that would have greatly increased her risk for stroke and even death.
"What scares me the most is, if she didn't come to me but instead, she found someone online to prescribe it for her, without knowing her full health history," Levy-Gantt said.
Patients assume the same treatment will work for them because a friend or celebrity on social media raved about it, she added.
Though she is open to considering options with more limited clinical evidence, Levy-Gantt tries to educate her patients about finding reputable sources of information.
 Monica Wang, ScD
Monica Wang, ScDPatient confusion about which health information to trust is understandable, according to Monica Wang, ScD, an associate professor of community health sciences at the Boston University School of Public Health in Massachusetts. Clinicians can acknowledge the deluge of information and ask patients about their current understanding of a particular topic or treatment. They might use plain English and culturally-appropriate language to dispel misinformation.
Tips for Primary Care Clinicians to Help Counter Menopause Misinformation
- Acknowledge to patients that you may not have all the answers; be willing to do follow-up research and have additional conversations as needed.
- Have a list of proven, scientifically-based, safe therapies to suggest and discuss.
- Ask for more details if a patient chooses to use a treatment based on influencer recommendations; review potential risks and encourage a follow-up visit after several months to assess efficacy and counsel them to stop if they are not improving or are experiencing adverse side effects.
- Share evidence-based plain-language books and articles with patients.
- Develop a simple fact sheet on various symptoms and treatments or use one from a credible source like The Menopause Society.
- Recommend several vetted user-friendly websites for more information about a specific symptom or condition.
- Suggest several social media menopause influencers whose messages are consistent with best practices.
- Don't write off menopause as simply a normal phase of life; regardless of age, clinicians should appropriately treat symptoms.
- Recognize your limitations; refer to a menopause specialist in your network when appropriate.
- Take continuing medical education courses, fill in knowledge gaps with additional reading, or consider becoming a certified menopause specialist.
Menopause influencers often promote expensive supplements or special diets, which are among the most common sources of health misinformation that circulates online, Wang said. Clinicians should tell patients to be wary about online promotion of supplements, especially if products are touted by a celebrity, if they are ordered from another country, or if the company does not state that it has safety or quality control measures.
Even therapies that seem healthy can be harmful if taken in large quantities or if a patient has an underlying condition. Misinformation or questionable solutions from other medical professionals is especially hard to dispel, Levy-Gantt said.
Green tea, known for its antioxidant properties and ability to reduce inflammation, can be helpful for some menopausal women. But consuming large doses of green tea extract, often sold in supplement form, has been linked to liver toxicity and liver failure. Some reports link black cohosh, a popular herbal remedy for hot flashes, to liver problems. Dong quai, a traditional Chinese medicine herbal remedy for hot flashes, should not be taken by women with fibroids, hemophilia, and other clotting problems, according to The Menopause Society.
Practice Active Listening
Women may find misinformation because they have symptoms that their primary care clinicians dismiss or ignore, according to Levy-Gantt. A good approach might be to ask what specifically caused them to want to try a particular solution. Then talk about those symptoms and figure out an individualized plan for their health needs on the basis of their health history.
 Jewel Kling, MD, MPH
Jewel Kling, MD, MPHJewel Kling, MD, MPH, chair of the Division of Women's Health Internal Medicine at Mayo Clinic in Scottsdale, Arizona, recommends that clinicians validate their patients' concerns. She keeps a list on hand of menopause influencers who are providing accurate information and tips because "there are some people that are doing a beautiful job," she said.
Physician-patient encounters are often subject to time constraints, but clinicians can continue conversations through follow-up visits or calls, portal messaging, or tap team members like nurses or physician assistants to schedule a separate consultation or message patients to respond to additional questions.
Mostly, just sit back and listen, Kling said.
"It doesn't have to take much time," she said. "But you're going to get so much information."
Liz Seegert is a freelance journalist.

.webp) 2 weeks ago
5
2 weeks ago
5




















 English (US)
English (US)