More than 1.3 million people are cared for in nursing homes each year. These individuals have complex health needs and often require skilled nursing care and rehabilitation services. Many are medically fragile and quite vulnerable to infection, as was made evident during the COVID-19 pandemic. Many of our currently available interventions to prevent the spread of multidrug-resistant organisms (MDROs) and MDRO infections are costly and challenging to implement, which can limit their effectiveness, particularly in the nursing home setting. Well-defined, evidence-based interventions, supported by data collected in nursing homes, are critical to protecting residents. The recently published PROTECT trial provides a relatively simple strategy to reduce infections, hospitalizations, and MDRO carriage among nursing home residents. Key takeaway points from this trial are provided below.
What is the PROTECT trial?
The PROTECT trial was a 28–nursing home pragmatic cluster-randomized trial jointly led by Loren G. Miller, MD, MPH, investigator at the Lundquist Institute for Biomedical Innovation and associate chief of infectious diseases at Harbor-UCLA Medical Center; and Susan Huang, MD, MPH, Chancellor's Professor in the Division of Infectious Diseases at the University of California, Irvine School of Medicine. UC Irvine is a Centers for Disease Control and Prevention (CDC) Prevention Epicenters Program partner, and CDC supports its work evaluating the use of chlorhexidine bathing to reduce harms from MDROs in nursing home residents.
The trial assessed whether a topical antiseptic soap and nasal ointment regimen given to all residents ("universal decolonization") could reduce infections, hospitalizations, and carriage of MDROs when compared with routine care. The "cluster-randomized" design meant that entire nursing homes, rather than individual residents, were randomly assigned to universal decolonization or routine care. This design allowed the evaluation of a quality improvement strategy that would be implemented across an entire nursing home. The trial involved nearly 14,000 residents who had an average age of 76 years and spent an average of 250 days in the nursing home. All 28 participating nursing homes were located in Southern California and provided skilled nursing and rehabilitative care.
How common were hospitalizations, infection-related hospitalizations, and MDROs in the nursing homes in the PROTECT trial at baseline?
Prior to the intervention assignment, the hospitalization rate in participating nursing homes was 3.5 per 1000 resident days. This represents approximately 10.5 residents per month being hospitalized for any reason in a usual nursing home with 100 residents. Overall, 62% of admissions were due to infection. This high rate of serious infection and hospitalization is exactly why the PROTECT trial was conducted.
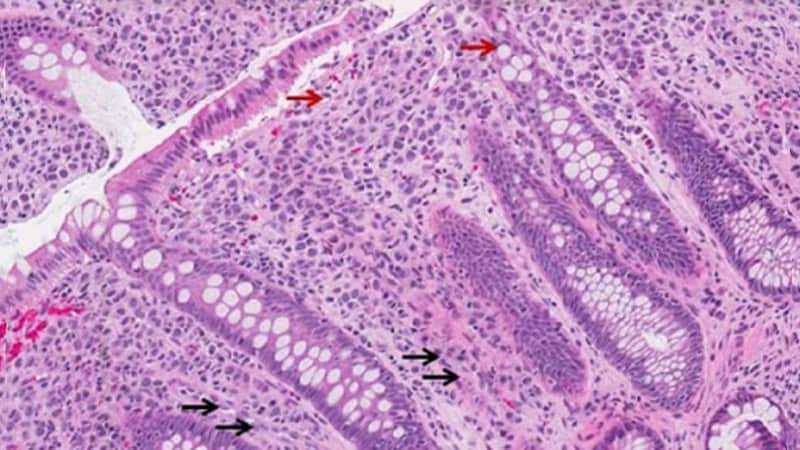
In addition, MDROs are common in nursing homes. On the basis of nasal and skin (axilla and groin) sampling in the PROTECT trial, half of residents had one or more MDROs. The most common MDROs were methicillin-resistant Staphylococcus aureus (MRSA; 37% carriage), extended-spectrum beta-lactamase producers (ESBL; 16%), and vancomycin-resistant Enterococcus (VRE; 6%). The high prevalence of MRSA was why an intervention strategy was selected that could reduce MRSA by decreasing carriage in the nose, the main reservoir for S aureus.
What intervention was studied in the PROTECT trial?
The 28 participating nursing homes were randomly assigned to one of two groups:
- Routine care (14 nursing homes)
- Universal decolonization (14 nursing homes)
Universal decolonization involved this process for all residents in the nursing home:
- Chlorhexidine antiseptic soap for all bathing and showering (typically 3x/week)
- 4% rinse-off solution for showering
- 2% leave-on solution for bed baths
- 10% povidone-iodine (iodophor) nasal swabs applied to both nostrils twice daily for 5 days for all new residents, and then twice daily Monday through Friday every other week for all residents.
What happened as a result of using chlorhexidine antiseptic soap and nasal povidone-iodine (iodophor)?
When compared with the routine-care group, these effects were found in the universal-decolonization group:
- The reasons for hospitalization changed. The rate of infection as a cause of hospitalization (primary outcome) was 17% lower. Among nursing home discharges, the rate of discharges to a hospital (secondary outcome) was 15% lower.
- When evaluating these same outcomes as a hospitalization rate per 1000 resident days, universal decolonization decreased infection-related hospitalizations by 31% per 1000 resident days, and it decreased any hospitalization by 18% per 1000 resident days.
- Overall, for a typical nursing home with 100 residents, where approximately 10.5 residents are hospitalized each month for any reason, universal decolonization prevented 1.9 infection-related hospitalizations per month per 100–occupied bed nursing home.
- The number needed to treat was 8.9 to prevent any hospitalization and 9.7 to prevent an infection-related hospitalization.
- The decolonization intervention also reduced MDRO prevalence by 30%. This included a 27% reduction in MRSA, a 50% reduction in ESBL, and a 71% reduction in VRE.
How does universal decolonization work, and is it safe?
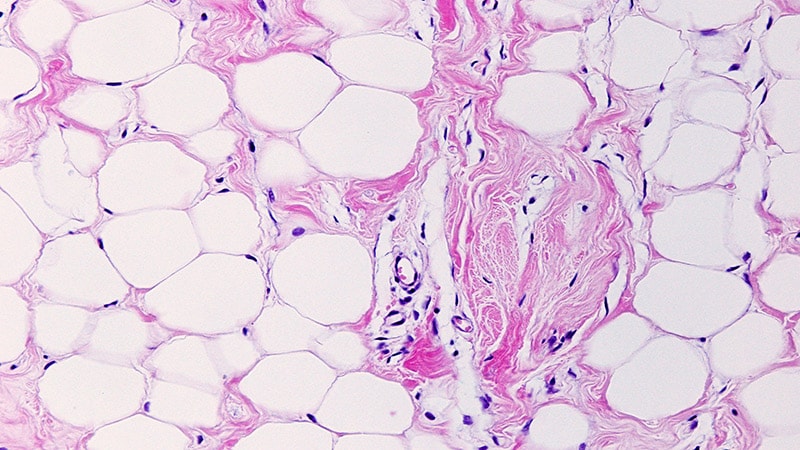
Universal decolonization works by reducing the amount of bacteria on the skin and in the nose during times when people are at high risk of developing infection from their own body bacteria. This includes times when patients are hospitalized or require nursing home support for performing daily hygiene needs and recovering from illness. It can be especially important when patients have antimicrobial-resistant bacteria; have lines, tubes, other medical devices; or have breaks in the skin or surgical incisions to protect. Nursing homes have a high proportion of residents who have antimicrobial-resistant bacteria on their bodies. Decreasing the amount of bacteria on the skin and in the nose may help reduce the spread of MDROs and other contagious pathogens within nursing homes.
- Mechanism of action:
- Chlorhexidine is a cationic surfactant that disrupts cell membranes. It is active against a wide range of microorganisms, including many multidrug-resistant bacteria. It binds to skin proteins and continues to kill germs on the skin for up to 24 hours. In a nursing home where bathing generally occurs three times per week, chlorhexidine reduced body bacteria and probably reduced the chance of recolonization.
- Povidone-iodine (iodophor) works by oxidizing proteins, nucleic acids, and fatty acids in microorganisms, leading to cell death. By applying it to the nose, it was used to reduce carriage of S aureus, both methicillin-sensitive (MSSA) and -resistant (MRSA) forms. The choice to use iodophor for 5 days every other week was based on data suggesting that nasal decolonization generally works for about 2 weeks before recolonization occurs.
- Safety profile: Both chlorhexidine and iodophor have been used safely in healthcare for over 60 years as topical antiseptics. In the PROTECT trial, among 7388 residents participating in the universal-decolonization intervention, there were 34 reports of skin irritation or allergy to chlorhexidine and one report of irritation or allergy to iodophor (0.4% adverse event rate). All side effects were mild, and residents discontinued the product in 26 cases.
Can nursing homes that adopt this strategy expect the same results?
The PROTECT trial was designed as a pragmatic trial. This meant that participating nursing homes carried out the assigned intervention using their own staff and usual operational oversight. Research staff provided nursing home leaders with educational materials, and supported training, feedback, and encouragement. Because of this, it would be reasonable to expect that nursing homes that dedicate leadership oversight to implementing the universal decolonization strategy as an important campaign can see similar results with training, monitoring, feedback, and encouragement.
Are there resources to help implement these findings?
These materials are available to aid with implementation:
- Free toolkit: A publicly available comprehensive toolkit involving protocols, training materials, posters, and frequently asked questions is available for download at Nursing Home Decolonization Toolkit | UCI Health | Orange County, CA
- Free training modules: Online learning modules to train certified nursing assistants and LPN/LVNs/RNs on how to perform chlorhexidine bathing are available from the National Association of County and City Health Officials (NACCHO). Modules are free but sign-up is required.
- Introductory video: A brief overview of the PROTECT trial is available.
Has this strategy been successful in other settings?
Yes. Large-scale randomized controlled trials have demonstrated the value of decolonization in several healthcare settings where patients are known to be at higher risk for infection. They include:
- Intensive care units (ICUs): Daily chlorhexidine bathing with and without 5 days of twice-daily mupirocin has been shown to prevent bloodstream infections and antimicrobial-resistant organisms when given to all ICU patients (universal decolonization). (See Related Reading below)
- Non-ICUs: Daily chlorhexidine bathing, plus an additional 5 days of twice-daily mupirocin for MRSA carriers, has been shown to reduce bloodstream infections and antimicrobial-resistant organisms in non-ICU patients with devices. (See Related Reading below)
- Post-discharge: Among MRSA carriers identified in the hospital, post-discharge use of a decolonization regimen twice monthly for 6 months was shown to reduce infections and hospitalizations due to any pathogen, as well as specifically due to MRSA, in the year following discharge. The regimen consisted of 5 days of chlorhexidine bathing plus twice-daily mupirocin.
Related Reading
Huang SS, Septimus E, Kleinman K, et al. Targeted versus universal decolonization to prevent ICU infection. N Engl J Med. 2013;368:2255-2265. Source
Climo MW, Yokoe DS, Warren DK, et al. Effect of daily chlorhexidine bathing on hospital-acquired infection. N Engl J Med. 2013;368:533-542. Source
Huang SS, Singh R, McKinnell JA, et al. Decolonization to reduce postdischarge infection risk among MRSA carriers. N Engl J Med. 2019;380:638-650. Source
Milstone AM, Elward A, Song X, et al. Daily chlorhexidine bathing to reduce bacteraemia in critically ill children: a multicentre, cluster-randomised, crossover trial. Lancet. 2013;381:1099-1106. Source
Huang SS, Septimus E, Kleinman K, et al. Chlorhexidine versus routine bathing to prevent multidrug-resistant organisms and all-cause bloodstream infections in general medical and surgical units (ABATE Infection trial): a cluster-randomised trial. Lancet. 2019;393:1205-1215. Source

.webp) 1 week ago
5
1 week ago
5























 English (US)
English (US)